Importance of Maintaining Routine and Consistency with Medication Regimen- specifically with Parkinson’s Disease
Written by: Erin Stosich, OTR/L, CLT, LSVT BIG certified, Goodcare AtHome Rehab Area Manager – Omaha
While there are various medications that can be taken to help manage symptoms of Parkinson’s Disease, Carbidopa-Levodopa is the most common. Levodopa is a medication that is absorbed by the body, transported to the brain, and converted into dopamine. It is paired with carbidopa to stop the conversion of levodopa to dopamine in the gut which can then lead to nausea. Dopamine is what your body uses to send messages between nerve cells. It is how your brain tells you to “lift your right arm” or “step with your left foot”. Depleted or low dopamine levels is one of the main factors of Parkinson’s Disease. Therefore, common symptoms are tremors, reduced motor control/coordination, stiffness and difficulty walking.
There are various forms of carbidopa-levodopa and unfortunately, they only last in the body for so long. Carbidopa-levodopa is typically dosed about 4 times a day. Because the medication is helping your body to produce dopamine, which helps exhibit more normal functioning, it is important to stick to your medication regimen as closely as possible. It is so easy in our busy lifestyles to “forget” to take our medications. With people who are living with Parkinson’s Disease, it sometimes becomes a caregiver’s responsibility to help administer meds. So, it is very important for not only the individual, but also the caregiver to understand the medication routine and always be prepared. When planning an outing, visiting family/friends, etc, always plan for medication times and have it along.
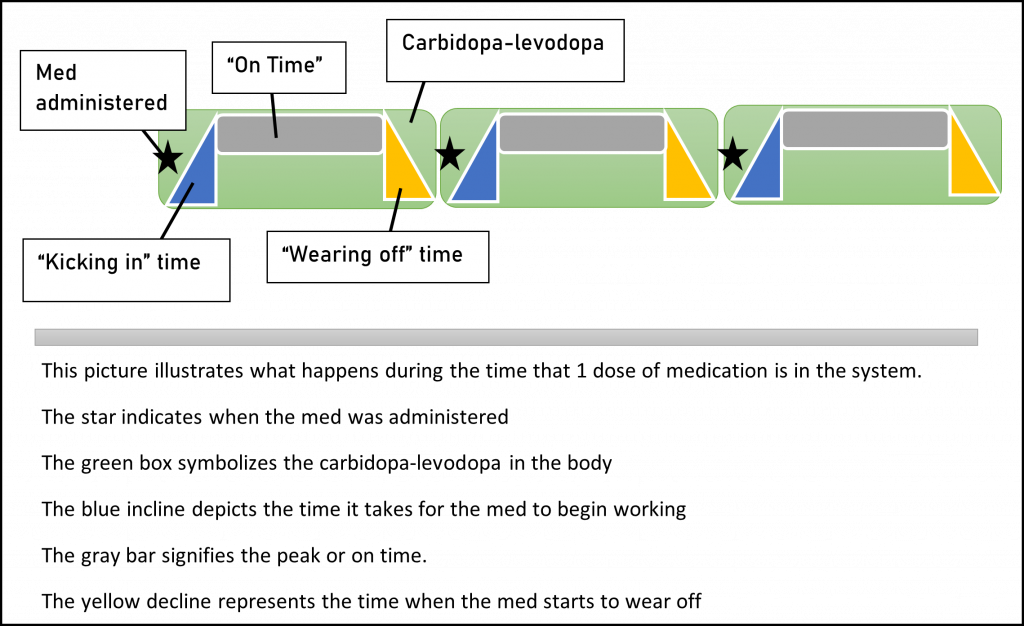
With the medication routine and dosage, there are periods of time referred to as “on times” and “off times”. These are durations when an individual is functioning fairly normal, and times when movements and tasks are more difficult. The regular administration of meds is what is going to help regulate those times and allow the individual and caregiver to plan accordingly. It is going to be much easier for the individual with Parkinson’s Disease to take a shower during an “on time” vs during a time when it is difficult to coordinate movements such as lifting their legs over the tub or walking in general. On the other side of that, people can also plan for the “off time”. Utilize that time to rest or complete smaller, less complex tasks. Below is a chart and a picture that help illustrate the on/off times during the day. The times of the chart are approximate and can vary in either direction depending on each individual along with their type of medication and dosage.
| 8:00 AM | Carbidopa-Levodopa |
| 8:00-8:30 | Med starting to work, symptoms begin to alleviate |
| 8:30-11:30 | Peak time; near normal function; “on time” |
| 11:30-12:00 | “wearing off time”; symptoms begin to reappear |
| 12:00 PM | Carbidopa-Levodopa |
| 12:00-12:30 | Med starting to work, symptoms begin to alleviate |
| 12:30-3:30 | Peak time; near normal function; “on time” |
| 3:30-4:00 | “wearing off time”; symptoms begin to reappear |
| 4:00 PM | Carbidopa-Levodopa |
| 4:00-4:30 | Med starting to work, symptoms begin to alleviate |
| 4:30-7:30 | Peak time; near normal function; “on time” |
| 7:30-8:00 | “wearing off time”; symptoms begin to reappear |
| 8:00 PM | Carbidopa-Levodopa |
| 8:00-8:30 | Med starting to work, symptoms begin to alleviate |
| 8:30-11:30 | Peak time; near normal function; “on time” |
| 11:30pm-8:00am | “wearing off time”; symptoms begin to reappear- however, most of the time is sleeping time; the morning time when you first wake up until that first dose kicks in will be the most difficult time of day |
As you can see, it is important to stick as closely as possible to the medication timing and routine. Just about that time when the medication will have worn off completely, another dose is due. If the medication routine is followed and the dosage is appropriate for the individual, the “down time” can be reduced to minimal amounts throughout the day and a majority of the time can be spent in “on times” where the individual can perform tasks with increased ease.
Another reason the medication routine is so important, is to help the doctor get a good understanding of how the medications are working. If the regimen is not followed, it will be very difficult for the doctor to adjust dosage and get the right meds to allow the individual to function at their maximum ability. It is very vital to note that every individual who lives with Parkinson’s Disease is different and there are also different stages of Parkinson’s Disease. Therefore, medications, techniques and strategies that work for one person, may not work for another. Always consult with your doctor and work together to determine the best treatment and routines for your individual needs.
Overall, this information is to help people with or without Parkinson’s Disease, have a better understanding of exactly how the medication works and why the regimen prescribed by the doctor is so important. This is in no way mean to replace any knowledge or recommendations that come from your personal doctor.
Occupational and Speech Therapists can assist with medication set-up. Strengthening may also help those with Parkinson’s Disease to increase everyday functioning. If you are interested in setting up a mobile outpatient evaluation with a Goodcare AtHome Rehab therapist call us at 605-231-2490 or email us at info@goodcareathomerehab.com.
